Are you looking for an essay on the ‘Immune Response and Its Types’? Find paragraphs, long and short essays on the ‘Immune Response and Its Types’ especially written for school and college students.
Essay # 1. Introduction to Immune Response:
The immune system protects the body from potentially harmful substances by recognizing and responding to antigens. Antigens are molecules (usually proteins) on the surface of cells, viruses, fungi, or bacteria. Non-living substances such as toxins, chemicals, drugs, and foreign particles (such as a splinter) can be antigens. The immune system recognizes and destroys substances that contain these antigens.
An immune response to foreign antigen requires the presence of an antigen-presenting cell (APC), (usually either a macrophage or dendritic cell) in combination with a B cell or T cell. When an APC presents an antigen on its cell surface to a B cell, the B cell is signaled to proliferate and produce antibodies that specifically bind to that antigen. If the antibodies bind to antigens on bacteria or parasites it acts as a signal for pmns or macrophages to engulf (phagocytose) and kill them.
Another important function of antibodies is to initiate the “complement destruction cascade.” When antibodies bind to cells or bacteria, serum proteins called complement bind to the immobilized antibodies and destroy the bacteria by creating holes in them. Antibodies can also signal natural killer cells and macrophages to kill viral or bacterial-infected cells.
If the APC presents the antigen to T cells, the T cells become activated. Activated T cells proliferate and become secretory in the case of CD4+ T cells, or, if they are CD8+ T cells, they become activated to kill target cells that specifically express the antigen presented by the APC. The production of antibodies and the activity of CD8+ killer T cells are highly regulated by the CD4+ helper T cell subset. The CD4+ T cells provide growth factors or signals to these cells that signal them to proliferate and function more efficiently. This multitude of interleukins or cytokines that are produced and secreted by CD4+ T cells are often crucial to ensure the activation of natural killer cells, macrophages, CD8+ T cells, and PMNs.
Essay # 2. Types of Immune Response:
a. Innate Immune Response:
The term, innate immunity, refers to the basic resistance to disease that a species possesses – the first line of defense against infection.
The characteristics of the innate immune response include the following:
i. Responses are Broad-Spectrum (non-specific)
ii. There is no memory or lasting protective immunity
iii. There is a limited repertoire of recognition molecules
iv. The responses are phylogenetically ancient.
Potential pathogens are encountered routinely, but only rarely cause disease. The vast majority of microorganisms are destroyed within minutes or hours by innate defenses. The acquired specific immune response comes into play only if these innate defenses are breached.
The elements of the innate immune response involves:
Anatomic Barriers:
A. Skin:
i. Epidermis – thin outer layer containing tightly packed epidermal cells and keratin (water -proofing) completely renewed every 15-30 days. Dermis – thicker inner layer contains sebaceous glands associated with hair follicles – produce sebum which consists of lactic and fatty acids maintaining a pH 3-5.
ii. Mucous membranes (ciliated epithelial cells; saliva, tears and mucous secretions) – GI, urogenital, respiratory tracts – collectively represents a huge surface area.
iii. Physiologic Barriers.
iv. Temperature – normal body temperature inhibits growth of most microorganisms.
v. Elevated body temperature (fever) can have a direct effect on pathogenic microorganisms.
vi. pH – low pH of stomach, skin, & vagina (inhibits microbial growth).
B. Chemical Factors:
i. Fatty acids, lactic acid
ii. Pepsin (digestive enzyme which hydrolyzes proteins)
iii. Lysozyme -hydrolytic enzyme found in mucous secretions – able to cleave the peti- doglycan layer of the bacterial cell wall
iv. Anti-microbial substances which directly destroy microorganims- cryptidins and a-defensins (produced in base of crypts of small intestine – damage cell membranes) b-defensins (produced within skin, respiratory tract – also damages cell membranes) surfactant proteins A & D (present in lungs – function as opsonins which enhance the efficiency of phagocytosis)
v. Interferons – group of proteins produced by cells following viral infection. Secreted by the cells, and then binds to nearby cells and induces mechanisms which inhibit viral replication.
vi. Complement – a group of serum proteins that circulate in an inactive proenzyme state. These proteins can be activated by a variety of specific and nonspecific immunologic mechanisms that convert the inactive proenzymes into active enzymes. The activated complement components participate in a controlled enzymatic cascade that results in membrane-damaging reactions which destroy pathogenic organisms by formation of a membrane attack comples (MAC).
C. Endocytic and Phagocytic Barriers:
Endocytosis is the process by which macromolecules contained within the extracellular tissue fluid are internalized by cells. Internalization occurs as small regions of the plasma membrane invaginate, or fold inward, forming small endocytic vesicles known as endosomes.
Occurs through pinocytosis or receptor-mediated endocytosis:
i. Pinocytosis – nonspecific membrane invagination
ii. Receptor-mediated endocytosis – specific, macromolecules are selectively internalized after binding to specific membrane receptors.
Following internalization, the endosomes fuse with primary lysosmes. Lysosomes contain large numbers of degradative enzymes (> 20 different hydrolytic enzymes including proteases, nucleases, lipases, etc.). The ingested macromolecules are subsequently digested into small breakdown products. Products not utilized by the cell are released through the process known as exocytosis.
Phagocytosis involves the ingestion of particulate material including whole pathogenic microorganisms. The plasma membrane expands around the particulate material to form large vesicles called phagosomes (10-20times larger than endosome). Only specialized cells are capable of phagocytosis, whereas endocytosis is carried out by virtually all cells. Once particulate matter is ingested into phagosomes, the phagosomes fuse with lysosomes and the ingested material is then digested by a process similar to that seen in endocytosis. The so- called “professional phagocytes” include- monocytes & macrophages, neutrophils, and dendritic cells.
Phagocytic cells distinguish between self and non-self by the recognition of common molecular pattern of the invading microorganisms.
This microbial pattern involves:
i. LPS- lipopolysaccharide (associated with the outer membrane of Gram – bacteria)
ii. Mannose, fucose, and other sugar residues (not just absence/presence but also factors like spacing between sugars on the cell surface)
iii. Teichoic acid (associated with the peptidoglycan cell wall of Gram+ bacteria)
iv. N-formyl peptides (recall that all prokaryotic protein sequences begin with a formyl- methionine)
These common microbial patterns are recognized by host proteins which have been termed as Pattern Recognition Molecules (PRMs) or Pattern Recognition Receptors (PRRs), which includes:
i. f-Met-Leu-Phe receptor (binds to N-formyl peptides, and when present attracts neutrophils)
ii. Complement receptors- designated CRs – (binds to complement components such as C3b and C4b which opsonize microorganims as a consequence of the activation of the complement cascade)
iii. Macrophage Mannose receptor (binds to mannose residues commonly present on surface of microorganisms)
iv. Scavenger Receptors – at least 6 different scavenger receptors with different specificities have been described (recognize certain anionic polymers and acetylated low- density lipoproteins)
v. CD14 (receptor on the surface of phagocytes which allows for the recognition of LPS)
The interaction between a PRM and its microbial pattern leads to a rapid cascade of events. Toll like receptors (TLR) were first identified in the fruitfly, Drosophila, and were shown to play a very important role in the development of the insect. More recently, toll receptors have been shown to also be involved in the innate immune response of fruit flies and other insects and even in vertebrate organisms including humans reported to possess several similar proteins.
TLR-4 plays an important role in signal transduction (transfer of the signal received at the cell membrane eventually to DNA sequences located in the nucleus of the cell). Importantly, TLR-4 is now known to activate a transcription factor known as NFkB.
NFkB activation eventually leads to transcriptional activation resulting in the synthesis of:
i. ROIs (Reactive oxygen intermediates) and RNIs (Reactive nitrogen intermediates) – highly toxic to microorganisms anti-microbial peptides (such as the defensins)
ii. Cytokines (the small proteins which function as the chemical messengers of the immune response facilitating cell-cell communication)
iii. Chemokines (small proteins which function in the chemotaxis of leucocytes) adhesion molecules (proteins which regulate the adhesive properties of leucocytes leading to alterations in leucocyte migration and trafficking)
iv. Acute phase proteins (proteins synthesized largely in the liver and secreted rapidly following infection or tissue injury).
b. Adaptive or Acquired Immune Response:
Natural immunity alone cannot protect the body from invading pathogens. Hence, immunity is provided by either stimulating an individual’s antibody production or by introducing antibodies acquired from other sources. Adaptive immunity involves the lymphocytes and develops as people are exposed to diseases or immunized against diseases through vaccination. The adaptive (or active) immunity, which develops throughout our lives and particularly, develops when a person is exposed to natural infection by pathogens or to some antigens in day-to-day life.
Following exposure, the immune system responds by producing specialized lymphocytes and special proteins called antibodies. Immunity of this kind lasts long in most cases. Immunity developed following clinical and sub-clinical infections also falls under this category. Artificially acquired active immunity arises from the stimulation of antibody production following the administration of specially prepared antigens called vaccines into the body by safe means.
This is termed as vaccination or active immunization. Vaccines are composed of inactivated bacterial toxins (toxoids), killed micro-organisms or living but attenuated (weakened) micro-organisms that are subjected to treatment wherein they lose their toxicity or the ability to cause a disease but are still capable of stimulating the immune system.
There are two fundamental adaptive mechanisms:
i. Cell-Mediated immunity and
ii. Humoral immunity.
i. Cell-Mediated Immunity:
In 1883 Elie Metchnikoff observed that blood cells also contribute to the immune system. He noted that some white blood cells were able to engulf invading micro-organisms, and he named these white blood cells as phagocytes. Macrophages engulf antigens, process them internally and then display parts of them on their surface together with some of their own proteins. This sensitizes the T cells to recognize these antigens. All cells are coated with various substances. CD stands for cluster of differentiation and there are more than one hundred and sixty clusters, each of which is a different chemical molecule that coats the surface. CD8+ is read “CD8 positive.” Every T and B cell has about 105 = 100,000 molecules on its surface. B cells are coated with CD21, CD35, CD40, and CD45 in addition to other non-CD molecules. T cells have CD2, CD3, CD4, CD28, CD45R, and other non-CD molecules on their surfaces.
The large number of molecules on the surfaces of lymphocytes allows a huge variability in the forms of the receptors. They are produced with random configurations on their surfaces. There are some 1018 different structurally different receptors. Essentially, an antigen may find a near-perfect fit with a very small number of lymphocytes, perhaps as few as one.
T cells are primed in the thymus, where they undergo two selection processes. The first positive selection process weeds out only those T cells with the correct set of receptors that can recognize the MHC molecules responsible for self-recognition. Then a negative selection process begins whereby T cells that can recognize MHC molecules complexed with foreign peptides are allowed to pass out of the thymus.
Cytotoxic or killer T cells (CD8+) do their work by releasing lymphotoxins, which cause cell lysis. Helper T cells (CD4+) serve as managers, directing the immune response. They secrete chemicals called lymphokines that stimulate cytotoxic T cells and B cells to grow and divide, attract neutrophils, and enhance the ability of macrophages to engulf and destroy microbes. Suppressor T cells inhibit the production of cytotoxic T cells once they are not needed, lest they cause more damage than necessary. Memory T cells are programmed to recognize and respond to a pathogen once it has invaded and has been thus repelled and neutralized.
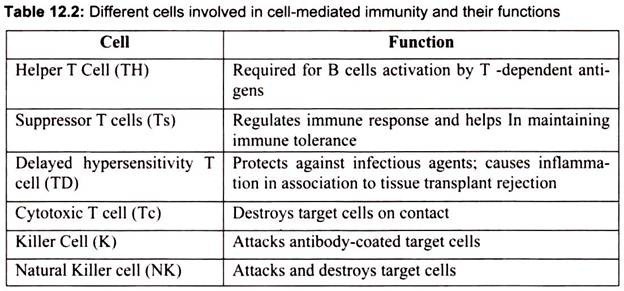
T cells, like B cells, have specificity for a single antigen indicating the presence of T cell receptors, which recognize the antigen. However, the response is not on the same line because being soluble antigens are unable to stimulate T cells as they cannot bind to T cells. A T cell responds only to those antigens processed by an antigen-presenting cell (APC). The major difference between T cell response and B cell response is that the T cell recognizes an antigen only when it is in close association with a major histocompatibility complex (MHC). This type of recognition is known as associative recognition. Various cells involved in cell mediated immunity are summarized in Table 12.2.
Once the APC is stimulated by an antigen, the cell secretes a substance called interleukin -1 (IL-I), a monokine secreted by macrophages, activates the T cell, which in turn begins to synthesize interleukin-2 (IL-2). The T cell also synthesizes surface receptors for IL-2. When the receptors bind to the IL-2, the T cells proliferate and differentiate into different effector cells, IL-2 receptors on T cells appear only if the T cell has been stimulated by an antigen.
ii. Humoral Immunity:
Emil von Behring and Shibasaburo Kitasato in 1890 demonstrated that serum from previously immunized animals, when administered to non-immunized animals, they got immunized. Since the immunity was mediated by antibodies contained in body fluids (in early days it was known as humors), this kind of immunity was named humoral immunity.
Humoral immunity or response is carried out by B cells, which produce antibodies. Humoral response is involved in the elimination of extracellular pathogens. It produces a large number of antibody molecules. B cells produced in the bone marrow mature and migrate into the Iymphoidal organs, where they encounter antigens.
When an appropriate antigen contacts the antigen receptor antibodies on a B cell, the latter proliferates into a large clone of cells. This phenomenon is known as clonal selection. Sometimes, the production of antibodies by a B cell depends on other cells, thus production of antibodies against T-dependent antigens requires the help of certain macrophages and T cells. The humoral immune system operates through antibodies found in blood plasma and lymph.
An immunocompetent but yet immature B-lymphocyte is stimulated to maturity when an antigen binds to its surface receptors and there is a T helper cell nearby (to release a cytokine). This sensitizes or primes the B cell and it undergoes clonal selection, and most of the family of clones becomes plasma cells. These cells, after an initial lag, produce highly specific antibodies at a rate of as many as 2000 molecules per second for four to five days. The other B cells become long-lived memory cells.
Antibodies, also called immunoglobulins or Igs (with molecular weights of 150-900 Md), constitute the gamma globulin part of the blood proteins. They are soluble proteins secreted by the plasma offspring clones of primed B cells.
The antibodies inactivate antigens by:
(a) Complement fixation (proteins attach to antigen surface and cause holes to form, i.e., cell lysis),
(b) Neutralization (binding to specific sites to prevent attachment,
(c) Agglutination (clumping),
(d) Precipitation (forcing insolubility and settling out of solution), and other more arcane methods.
Constituents of gamma globulin are:
IgG-76%, IgA-15%, IgM-8%, IgD-1%, and IgE- 0.002% (responsible for autoimmune responses, such as allergies and diseases like arthritis, multiple sclerosis, and systemic lupus erythematosus). IgG is the only antibody that can cross the placental barrier to the fetus and it is responsible for the 3 to 6 month immune protection of newborns that is conferred by the mother. IgM is the dominant antibody produced in primary immune responses, while IgG dominates in secondary immune responses. IgM is physically much larger than the other immunoglobulins.
The upper part or Fab (antigen binding) portion of the antibody molecule (physically and not necessarily chemically) attaches to specific proteins (called epitopes) on the antigen. Thus antibody recognizes the epitope and not the entire antigen. The Fc region is crystallizable and is responsible for effector functions, i.e., the end to which immune cells can attach. In addition to these antibody produced, it has been found that the B cells can produce as many as 1014 conformationally different forms.
All of these mechanisms hinge on the attachment of antigen and cell receptors. Since there are many receptor shapes available, WBCs seek to optimize the degree of confluence between the two receptors. The number of these “best fit” receptors may be quite small, even as few as a single cell. This attests he specificity of the interaction. Nevertheless, cells can bind to receptors whose fit is less than optimal when required. This is referred to as cross- reactivity.
Regulation of the Humoral Response:
Immune responses are tightly regulated complex interaction of cells and mediators and operate through a mechanism that prevents anti self-reactivity. Regulation of the immune response is possibly mediated in several ways. First, a specific group of T-cells, suppressor T- cells, are thought to be involved in turning down the immune response. Like helper T-cells, suppressors T-cells are stimulated by antigen but instead of releasing lymphokines that activate B-cells (and other cells), suppressor T-cells release factors that suppress the B-cell response. While immunosuppression is not completely understood, it appears to be more complicated than the activation pathway, possibly involves additional cells in the overall process.
Other means of regulation involve interactions between antibody and B-cells. One mechanism, “antigen blocking”, occurs when high doses of antibody interact with all of the antigenic epitopes, thereby inhibiting interactions with B-cell receptors. A second mechanism, “receptor cross linking”, results when antibody, bound to a B-cell via its Fc receptor and the B-cell receptor both combine with antigen. This “cross-linking” inhibits the B-cell from producing further antibody.
Another means of regulation that has been proposed is the idiotypic network hypothesis. This theory suggests that the idiotypic determinants of antibody molecules are so unique that they appear foreign to the immune system and are, therefore, antigenic. Thus, production of antibody in response to antigen leads to the production of anti-antibody in response, and anti-anti-antibody and so on. Eventually, however, the level of [anti]n-antibody is not sufficient to induce another round and the cascade thus ends.
Passive Immunity:
Passive immunity is the immunity acquired by the transfer of antibodies from another individual, as through injection or placental transfer to a fetus. Protection from passive immunity diminishes in a relatively short time, usually a few weeks or months. Infants have passive immunity because they are born with antibodies that are transferred to them through the placenta from the mother. These antibodies disappear between 6 and 12 months of age.
Here, the fetus is immune to those diseases to which the mother is immune, but only for a short period. For example, if the mother is immune to diphtheria, chicken pox, and polio, the newborn is also immune to the same diseases but only for a period not exceeding six months. Similarly, certain amount of immunity is provided through breast-feeding. Certain antibodies can pass from the mother to the infant via the breast milk.
Passive immunization involves injection of antiserum, which contains antibodies that are formed by another person or animal. It provides immediate protection against an antigen, but does not provide long-lasting protection. Gamma globulin (given for hepatitis exposure) and tetanus antitoxin are examples of passive immunization. These antibodies are produced either in animals or humans and then administered to the subject.